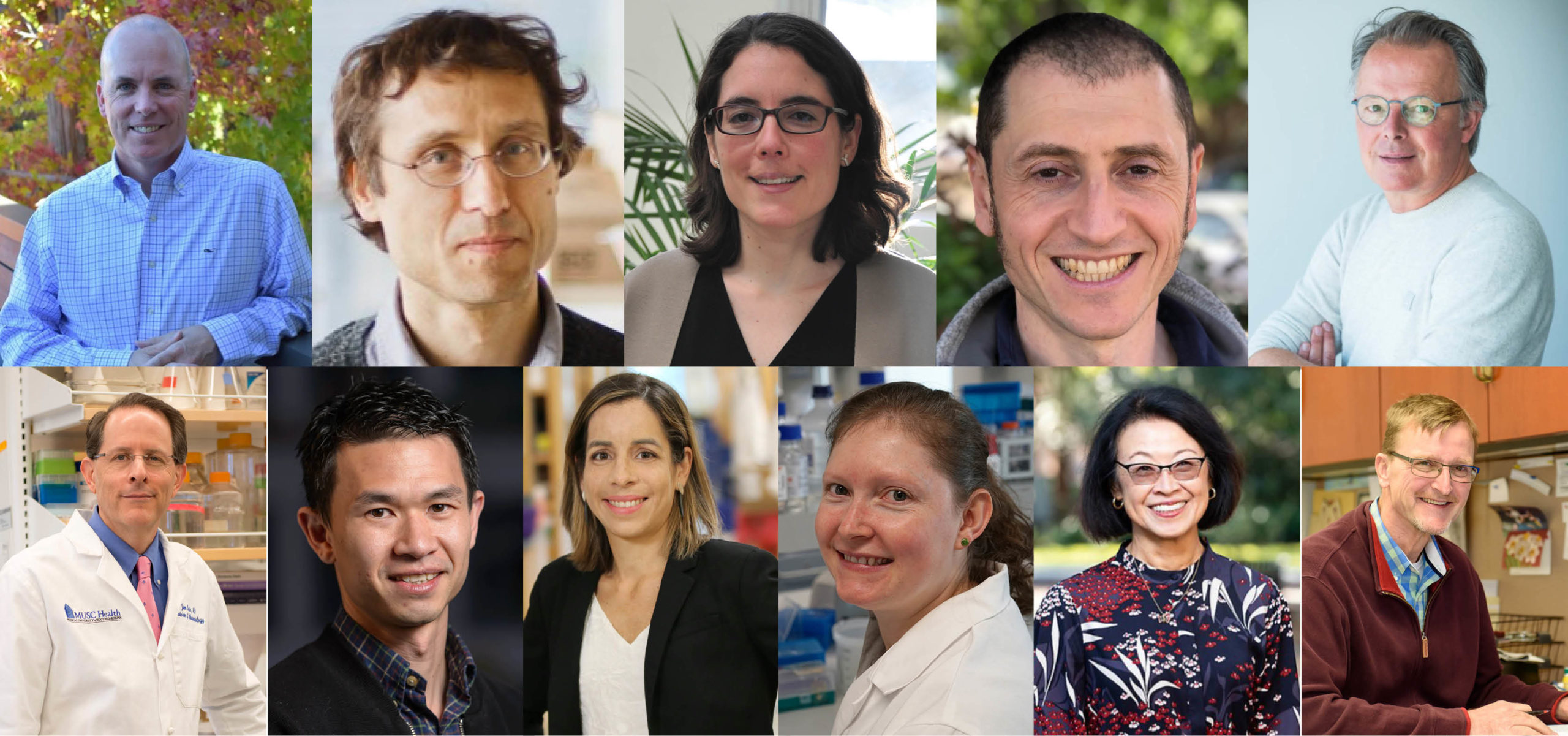
NEW YORK, NY, December 14, 2021. The Lupus Research Alliance proudly announced today recipients from the U.S. and around the world of the 2021 Lupus Innovation Award which will fund wide ranging areas of research from probing the development and progression of lupus to pointing to potential personalized therapies.
The Lupus Innovation Award provides support for highly innovative approaches to major challenges in lupus research with a special emphasis on exploring fundamental mechanisms, novel targets for drug development, novel technologies, and interdisciplinary approaches. The Award offers up to $150,000/year total costs for up to two years, and early-stage investigators are eligible for an additional year of funding upon successful completion of the original grant. These are investigators who are in the early stages of their research career.
Three of the projects intend to illuminate the genetic causes of lupus which are still incompletely understood. The other eight studies aim to develop personalized medicine approaches for lupus patients – either by maximizing the effectiveness while minimizing side effects of existing immunosuppressive drugs or by laying the foundation for brand new therapeutics.
Three Researchers Probing Genetic Causes of Lupus
Gregory Barton, PhD; University of California, Berkeley
Dr. Barton previously identified 20 genes in mice that push an important molecule called Toll-like receptor 7 or TLR7 to promote immune responses against the body’s own genetic material, which leads to lupus. Using this grant, he will study how the genes he identified, when turned “off”, influence TLR7 and how these genes, when turned “off”, promote lupus in mice.
Jason Cyster, PhD; University of California, San Francisco
Dr. Cyster will look at a specific protein, P2RY8, found on the surface of B cells to see if its loss leads B cells to produce autoantibodies, which results in lupus development or increased disease severity. Using human blood and tissue samples, he will see what percentage of the patient population have a mutation in this protein to see if it is a genetic cause of lupus.
Maria Gutierrez-Arcelus, PhD; Boston Children’s Hospital, Boston, Massachusetts
Dr. Gutierrez-Arcelus and her team will use the latest state-of-the-art technology to compare genetic material (RNA) and proteins in B cells from both healthy individuals and lupus patients. This grant will be used to study how underlying genetic changes in two important human B cell molecules (B cell receptor and TLR7) affect human B cell function and influence the different lupus symptoms that are seen in the clinic.
Personalized and Precision Medicine Approaches in Lupus
Nunzio Bottini, MD, PhD; University of California, San Diego, California
Dr. Bottini aims to reduce lupus symptoms while leaving the important infection-fighting components of the immune system intact. To do this, he will study if turning “on” a specific molecule called PTPRS in plasmacytoid dendritic cells, immune cells that fight viruses and bacteria in healthy people, causes these cells to produce less type I interferons that cause inflammation.
Bart Lambrecht, MD, PhD; VIB-UGent Center for Inflammation Research, Ghent, Belgium
Dr. Lambrecht and his team will study how IgA, a specific type of antibodies, influence lupus nephritis. Lupus patients have disturbances in their microbiome – the trillions of micro-organisms that live in and on the human body – and this might be the cause of alterations in IgA antibodies in lupus patients. Thanks to this grant, they are able to study how the microbiome modulates IgA in lupus, and how IgA affects lupus severity. Dr. Lambrecht seeks to identify single strains of bacteria that may increase or decrease lupus disease activity, which could result in novel therapies for lupus patients.
James Oates, MD; Medical University of South Carolina, Charleston, South Carolina
Dr. Oates found that kidney disease in a mouse model of lupus is worse when endothelial cells, the cells that line the blood vessels, fail to protect blood vessels from factors causing inflammation, which leads to endothelial dysfunction. Using this grant, he will now test if sepiapterin, an existing medication shown to improve endothelial dysfunction in diabetes, restores the protective role of endothelial cells and decreases kidney inflammation in mice with lupus nephritis.
Joshua Ooi, PhD; Monash University, Melbourne, Australia
Dr. Ooi developed specialized regulatory T cells which suppress the misguided immune response that leads to lupus nephritis. He will produce and test the effectiveness of “clinical-grade” regulatory T cells on lupus nephritis patients’ immune cells as well as in mice with lupus nephritis. This study could lead to a potential new treatment approach for lupus nephritis.
Zaida Ramirez-Ortiz, PhD; University of Massachusetts Chan Medical School, Worcester, Massachusetts
Dr. Ramirez-Ortiz previously discovered that immune cells that consume dysfunctional, dying or dead cells, called phagocytes, have a receptor molecule SCARF1 on their cell surface that is responsible for detecting and removing the dead cells. With this grant, Dr. Ramirez-Ortiz will compare SCARF1 on phagocytes from lupus patients to those from healthy people. She will also examine blood samples from lupus patients to see if they produce autoantibodies against SCARF1.
Joanne Reed, PhD; Westmead Institute for Medical Research, Westmead, Australia
Dr. Reed will study how the immune cells responsible for making the autoantibodies that attack the kidneys develop, and learn how they are different from the normal and healthy B cells which produce antibodies to fight infection. This work will be done using new state-of-the-art technology that looks at single B cells responsible for producing disease-causing autoantibodies.
Betty Tsao, PhD; Medical University of South Carolina, Charleston, South Carolina
Dr. Tsao previously identified a defect in a gene called SAT1 that may be associated with lupus in children, especially in boys. Using mouse models, she will investigate how this defective gene could disturb metabolism and function of immune cells, leading to the development of lupus at a young age. She will test natural compounds to see if they reverse this metabolism defect.
Lonnie Wollmuth, PhD; Stony Brook University, Stony Brook, New York
Dr. Wollmuth will develop strategies targeting the NMDA receptor, a molecule that controls communication between nerve cells to prevent or reduce brain disorders in lupus patients. Using mouse models, the research team will first look at the damage caused by individual antibodies targeting the NMDA receptor, and then see if the damage can be blocked by various agents.
Collectively, these 11 projects explore multiple components of lupus, with a focus on the cause of lupus as well as more personalized and precision medicine approaches to lupus treatments. Lupus has a broad range of causes and symptoms. Studying the disease from different vantage points can maximize the overall understanding of the disease, which can lead to more viable treatment options.
Lupus Research Alliance Chief Scientific Officer Dr. Teodora Staeva said, “We are proud to support fundamental lupus research through these grants, in order to encourage the development of novel and/or improved therapeutic options for the lupus patient community.”
About Lupus
Lupus is a chronic, complex autoimmune disease that affects millions of people worldwide. More than 90 percent of people with lupus are women; lupus most often strikes during the childbearing years of 15-45. African Americans, Latinx, Asians and Native Americans are two to three times at greater risk than Caucasians. In lupus, the immune system, which is designed to protect against infection, creates antibodies that can attack any part of the body including the kidneys, brain, heart, lungs, blood, skin, and joints.
About the Lupus Research Alliance
The Lupus Research Alliance is the largest non-governmental, non-profit funder of lupus research worldwide. The organization aims to transform treatment by funding the most innovative lupus research, fostering diverse scientific talent, and driving discovery toward better diagnostics, improved treatments and ultimately a cure for lupus. Because the Lupus Research Alliance’s Board of Directors funds all administrative and fundraising costs, 100% of all donations goes to support lupus research programs.
# # #
Tags: Bart Lambrecht, James Oates, Joanne Reed, Betty Tsao, Lonnie Wollmuth, Joshua Ooi, Zaida Ramirez-Ortiz, Lupus Innovation Award, Gregory Barton, Dr. Jason Cyster, Dr. Maria Gutierrez-Arcelus, Nunzio Bottini