LRA-Supported Researcher Finds Similarity between COVID-19 and Lupus Flares
LRA-Supported Researcher Finds Similarity between COVID-19 and Lupus Flares
October 21, 2020
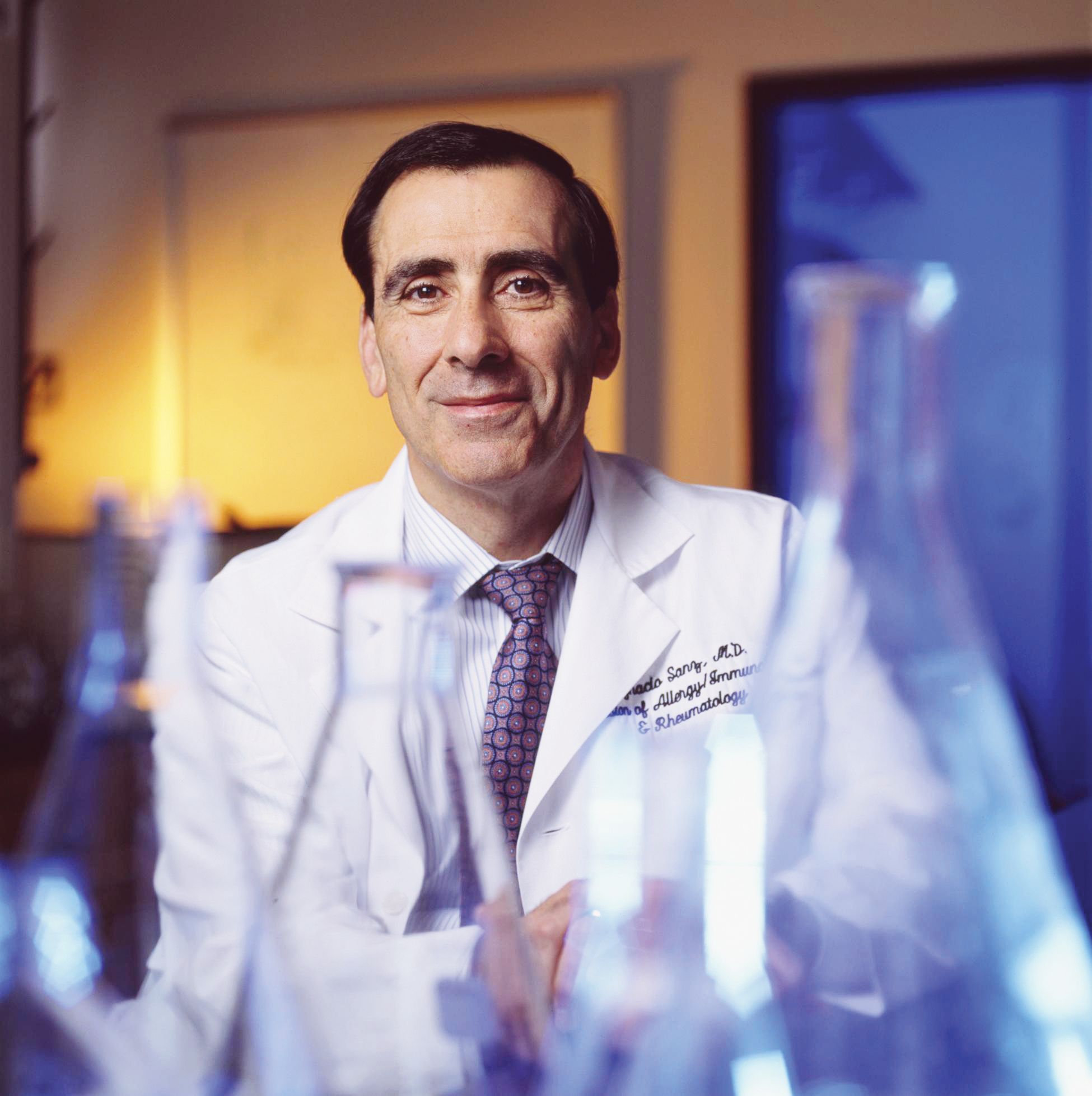
In a recent study published in Nature Immunology, LRA Lupus Insight Prize recipient Dr. Ignacio Sanz and colleagues found that the immune response in patients hospitalized with severe COVID-19 was different from that in patients with mild disease, and that the immune response in severely ill COVID-19 patients was more like a lupus flare. They saw that among severely ill COVID-19 patients, some immune cells called B cells reproduced unchecked, and were linked to an overactive immune response. This immune response was seen in the most severely ill COVID-19 patients, suggesting that it may be harmful to the COVID-19 patients. If this immune response persists, patients who survive severe COVID-19 may risk going on to develop autoimmune disease. These findings may allow researchers to better understand how autoimmune diseases like lupus develop after severe infections.
B cells are important cells of the immune system that help the body attack viruses and bacteria by smothering them with antibody proteins. Other cells of the immune system known as T cells “help” the good B cells reproduce and kill misbehaving B cells that would attack the body. T cells identify the good B cells and promote B cell survival in specialized locations called lymph node follicles. But during strong inflammatory responses, B cells can also reproduce and make antibodies outside the follicles. These kinds of B cells found outside of lymph node follicles are known as extrafollicular B cells.
Previous research by Dr. Sanz found that there are more of these extrafollicular B cells that escape T cell attention during lupus flares. This allows harmful B cells that could attack the body to quickly reproduce. Recent studies have revealed differences between the B cells of COVID-19 patients with mild and severe disease. In patients with severe illness, B cells quickly reproduce and release large amounts of antibodies. In contrast, patients with mild illness have a longer delay in the B cell response and produce fewer antibodies.
Due to the importance of B cells in fighting COVID-19, this study compared B cells from patients with mild and severe disease to healthy donors. The B cell response in COVID-19 patients was also compared to B cells from patients with active lupus.
Using a highly specialized technique called flow cytometry, Dr. Sanz and his colleagues were able to find extrafollicular B cells. The team found that COVID-19 patients with severe illness had many more extrafollicular B cells compared to patients with mild illness as well as healthy donors. In fact, these COVID-19 patients had as many extrafollicular B cells as had been seen in patients with active lupus. This suggests that similar mechanisms underlie the immune response during severe COVID-19 and lupus flares. Measuring the levels of these expanded extrafollicular B cells may allow identification of patients with overactive immune responses to COVID-19 and help guide their treatment.
Dr. Sanz’s findings help improve the understanding of the immune response during lupus. They may also partly explain how autoimmune disease arises in lupus patients. This work was enabled by support from the LRA and the NIAID Emory Autoimmunity Center of Excellence.