Researchers Discover How Gut Bacteria Can Trigger Autoimmunity
Researchers Discover How Gut Bacteria Can Trigger Autoimmunity
August 4, 2022
Immunologists have found that a certain gut bacteria escapes from the intestines to trigger inflammation that can lead to autoimmune diseases. A new study published in Nature provides an insight into how particular gut bacteria evolve over time through a phenomenon called ‘within-host evolution’. The new findings open the door for the development of personalized treatments for autoimmune diseases, including lupus.
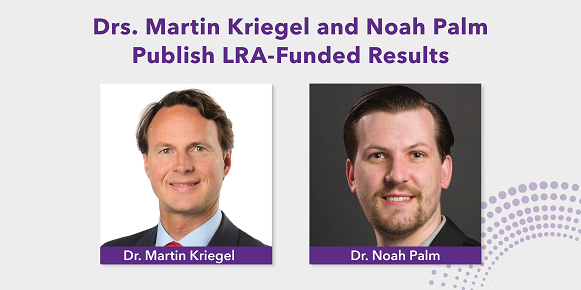
This research was partly funded by the Lupus Research Alliance through the Lupus Insight Prize awarded to Martin Kriegel, MD, PhD, Professor at the Institute of Musculoskeletal Medicine at the University of Münster, Germany and Associate Professor Adjunct of Immunobiology and of Medicine at Yale University School of Medicine.
Gut microbiota (commensal bacteria) are microbes that live within the intestines. Hundreds of different types of bacteria make up what is known as the commensal microbiome that populates the intestines of every human. Most bacterial species living in the human gut support good health. However, some bacteria with the potential to become harmful – pathobionts – have been linked to the development of various chronic diseases, including lupus and inflammatory bowel disease.
Dr. Kriegel was the first to identify that a particular pathobiont, Enterococcus gallinarum, breaks through the gut lining and enters the liver and lymph nodes, triggering the production of antibodies against the body’s own tissues – autoantibodies – and causing immune cell overactivation. Dr. Noah Palm, who is an Associate Professor of Immunobiology at Yale University School of Medicine, together with critical input from Dr. Kriegel, further built upon the initial discovery to understand how pathobionts cause autoimmunity and discovered within-host evolution as an unexpected and new mechanism.
Dr. Palm`s research team used Enterococcus gallinarum in mice, in combination with an advanced research approach known as comparative genomics, to discover that this particular pathobiont can develop changes in its genetic makeup. As a result, Enterococcus gallinarum can diverge into two distinct populations inside the mouse gut, with one group remaining harmless while the other population acquired the ability to escape from the gut and move into the liver and lymph nodes. While the immune system in healthy people detects pathogens and removes them, Enterococcus gallinarum remains partly hidden from the immune system in the lymph nodes and liver, causing inflammation to simmer below the surface for a long time before symptoms of an autoimmune disease such as lupus or autoimmune liver disease develop. Because pathobionts can move into tissues and organs outside the gut long before an autoimmune disease develops, this new finding also sheds light on why risk of illness increases with age.
“These groundbreaking findings provide new opportunities to develop treatments for autoimmune diseases, including lupus. One could envision new personalized therapies that would involve limiting the within-host evolution of bacteria and their escape from the human gut,” explained Dr. Kriegel.
“Many unanswered questions remain, including why this process causes disease in some people but not everyone,” noted Dr. Palm. “Because pathobionts evolve differently in each person, one answer may be that environmental factors such as a healthy diet promote diverse bacterial communities where numerous commensal microbes compete for space. Since not all commensal bacteria have the ability to escape from the gut, the diversity of bacteria living in the gut could decrease the likelihood that a single pathobiont will acquire the ability to translocate and drive the development of inflammatory disease.”