Lupus Research Alliance Announces Four New Recipients of the Lupus Mechanisms and Targets Award
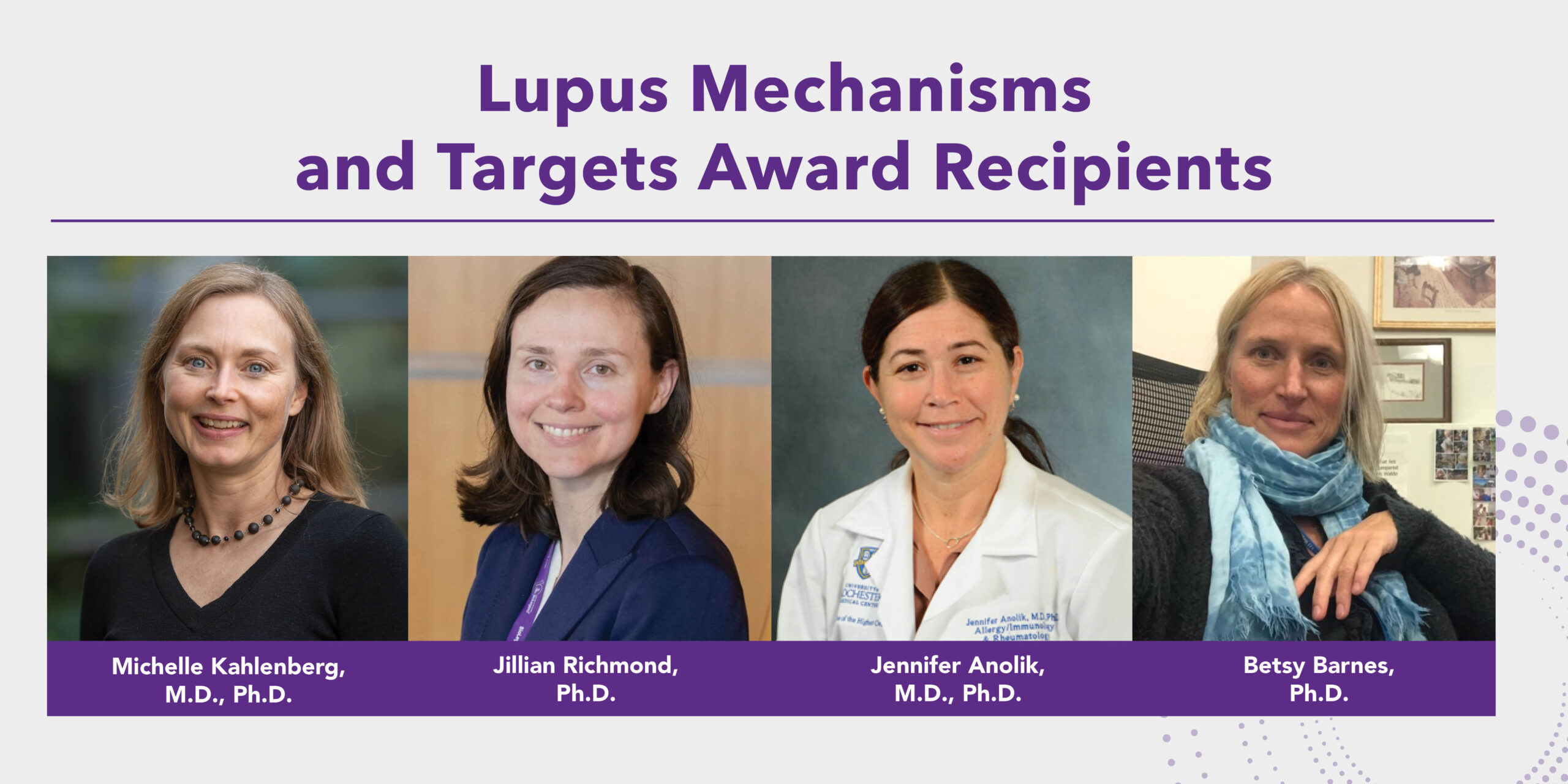
Lupus Research Alliance Announces Four New Recipients of the Lupus Mechanisms and Targets Award
Winning projects will explore new potential treatment approaches to prevent lupus from developing or prevent or slow disease progression.
NEW YORK, NY, April 20, 2023. The Lupus Research Alliance (LRA) today announced the newest Lupus Mechanisms and Targets Award grant recipients. The winning four projects collectively test potential treatment approaches to prevent lupus from developing or reducing lupus disease activity. Lupus has a broad range of causes and symptoms, and these multiple approaches are important for designing customized therapies that can provide better outcomes for a wide range of patients.
The LRA LMTA grants offer up to $600,000 over three years for research focusing on investigating molecular pathways or targets leading to the development of new or improved therapies for patients with cutaneous and systemic lupus erythematosus (SLE).
“These four new LMTA awards support innovative lupus researchers whose work is poised to deliver much needed new information for the lupus field. We are proud to be able to offer this financial support, with the ultimate goal of improving outcomes for lupus patients,” said Teodora Staeva, Ph.D., vice president and chief scientific officer of LRA.
Lupus Mechanisms and Targets Award Winners
Jennifer Anolik, M.D., Ph.D.; University of Rochester Medical Center
Dr. Anolik will investigate if sodium-glucose cotransporter-2 (SGLT2) inhibitors – a class of drugs approved to treat type 2 diabetes and associated kidney disease – can improve outcomes in lupus nephritis, which is inflammation in the kidneys caused by lupus that affects 40 to 70 percent of lupus patients. Current treatment approaches target inflammation with little impact on fibrosis and injury. Dr. Anolik will study mice with lupus nephritis to see if SGLT2 inhibitors reduce kidney hypoxia, inflammatory CD8 T cells, and kidney injury. She will also begin to investigate the effects of treatment with SGLT2i on clinical outcomes and pathogenic CD8 T cells in the blood and urine of patients with lupus nephritis.
Betsy Barnes, Ph.D.; The Feinstein Institutes for Medical Research
Systemic lupus erythematosus (SLE) has heritable components that can be passed on to children through gene variants. Variants in the interferon regulatory factor 5 (IRF5) gene, which controls the production of type I interferons, can be inherited, and they increase the risk of developing SLE. Dr. Barnes has recently identified a new regulator of IRF5 function– STK25 – that turns on IRF5 in SLE immune cells. Using this award, Dr. Barnes will compare STK25 activity in healthy people with and without IRF5 gene variants and in SLE patients. She will also aim to determine how STK25 activates IRF5 in response to SLE triggers and investigate if loss of the STK25 gene protects against lupus in lupus-prone mice, which will aid future clinical trials focused on targeting STK25 and/or IRF5 as new therapeutics.
Michelle Kahlenberg, M.D., Ph.D.; University of Michigan
Dr. Kahlenberg recently found that abnormal activity of Hippo proteins turns on the overproduction of immune system molecules (interferons) in lupus patients’ blood and skin. Dr. Kahlenberg will use this award to study whether turning off these Hippo proteins will decrease the amount of type I interferons, one of the hallmarks of cutaneous lupus and SLE. Her investigation will determine if Hippo proteins could serve as new therapeutic targets. Dr. Kahlenberg’s work builds on decades of pioneering studies on type I interferons funded by the LRA.
Jillian Richmond, Ph.D.; University of Massachusetts Chan Medical School
T cells are immune cells that can cause lupus flares in the skin. Dr. Richmond found that skin T cells in both people and mice have a protein on their cell surface called CXCR6. The T cell CXCR6 interacts with a protein called CXCL16 on skin cells, similar to how a lock and key fit together. Dr. Richmond will use this award to determine if the CXCL16-CXCR6 interaction is important in keeping the harmful T cells in the skin of patients with cutaneous lupus. She will also investigate if targeting these two molecules will provide a lasting treatment response in pet dogs with skin lupus through a veterinary clinical trial. This project could provide new information about the molecules on the surface of lupus-causing immune cells that could be targeted to prevent or slow lupus disease progression.
About Lupus
Lupus is a chronic, complex autoimmune disease that affects millions of people worldwide. More than 90 percent of people with lupus are women; lupus most often strikes during the childbearing years of 15-45. African Americans, Hispanic/Latino, Asians and Native Americans are two to three times at greater risk than Caucasians. In lupus, the immune system, which is designed to protect against infection, creates antibodies that can attack any part of the body including the kidneys, brain, heart, lungs, blood, skin, and joints.
About the Lupus Research Alliance
The Lupus Research Alliance is the largest non-governmental, non-profit funder of lupus research worldwide. The organization aims to transform treatment by funding the most innovative lupus research, fostering diverse scientific talent, and driving discovery toward better diagnostics, improved treatments and ultimately a cure for lupus. Because the Lupus Research Alliance’s Board of Directors funds all administrative and fundraising costs, 100% of all donations goes to support lupus research programs.