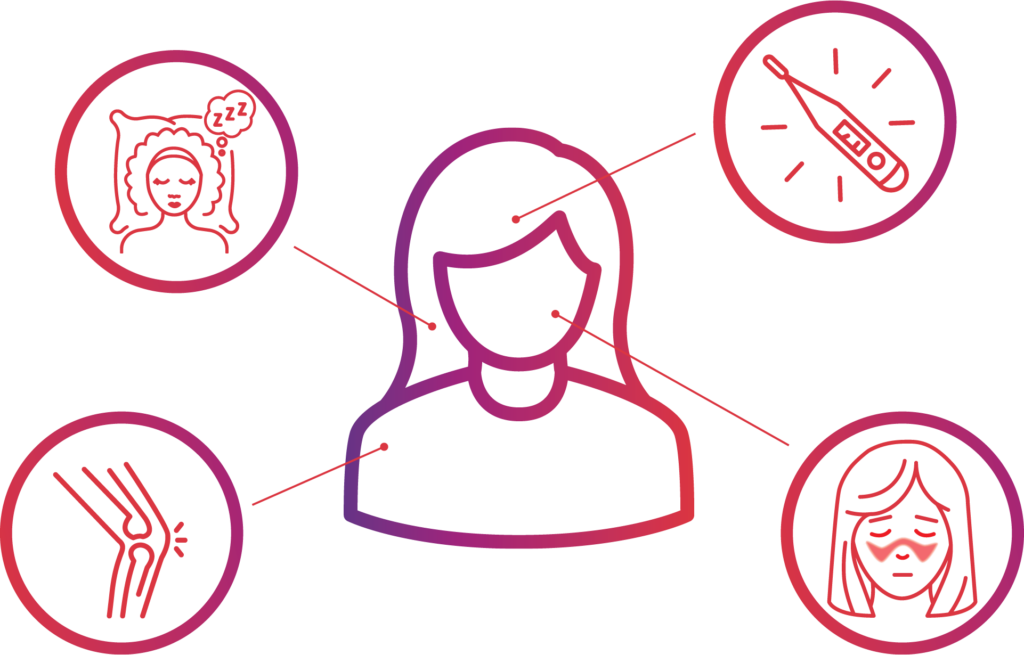
The most common symptoms of lupus are extreme fatigue, skin rashes, joint pain and unexplained fevers.
Contact Lupus Research Alliance Today
Common Symptoms of Lupus
Lupus Fatigue

Approximately 50%–90% of people with lupus identify fatigue as one of their primary symptoms. A number of factors can contribute to fatigue in lupus, including the disease itself, psychological factors, lifestyle factors, and medications.
No matter the cause, it’s clear that fatigue can significantly impact patients’ quality of life, including lessening the ability to function at home and at work.
 Malar Rash (Butterfly Rash)
Malar Rash (Butterfly Rash)
About half of people with lupus experience a characteristic red “malar” rash or color change that may appear across the cheeks and bridge of the nose in the shape of a butterfly. The rash can last from days to weeks and is sometimes painful or itchy. Rashes may also occur on the face and ears, upper arms, shoulders, chest, hands and other areas exposed to the sun.
Sun Sensitivity (Photosensitivity)
Because many people with lupus are sensitive to sunlight (called photosensitivity), skin rashes often first develop or worsen after being out in the sun. Some people find that the appearance of the butterfly rash is a sign of an oncoming disease flare.
Joint Pain and Swelling (Arthritis)
 Up to 90% of people with lupus will have arthritis, which is defined as inflammation or swelling of the joint lining. The most common symptoms of arthritis are stiffness and aching, most often in the hands and wrists. Symptoms of arthritis can come and go and move from one joint to another. Pain and stiffness tend to be worse in the morning and improve as the day goes on. People with lupus can also experience pain in the joints without swelling or tenderness, which is referred to as arthralgia.
Up to 90% of people with lupus will have arthritis, which is defined as inflammation or swelling of the joint lining. The most common symptoms of arthritis are stiffness and aching, most often in the hands and wrists. Symptoms of arthritis can come and go and move from one joint to another. Pain and stiffness tend to be worse in the morning and improve as the day goes on. People with lupus can also experience pain in the joints without swelling or tenderness, which is referred to as arthralgia.
 Fever
Fever
Most people with systemic lupus erythematosus (SLE) experience unexplained fevers (temperatures over 100°F (37.8°C). Physicians may recommend acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as naproxen or ibuprofen.
Lupus Complications